ALS & Breathing
How ALS affects breathing
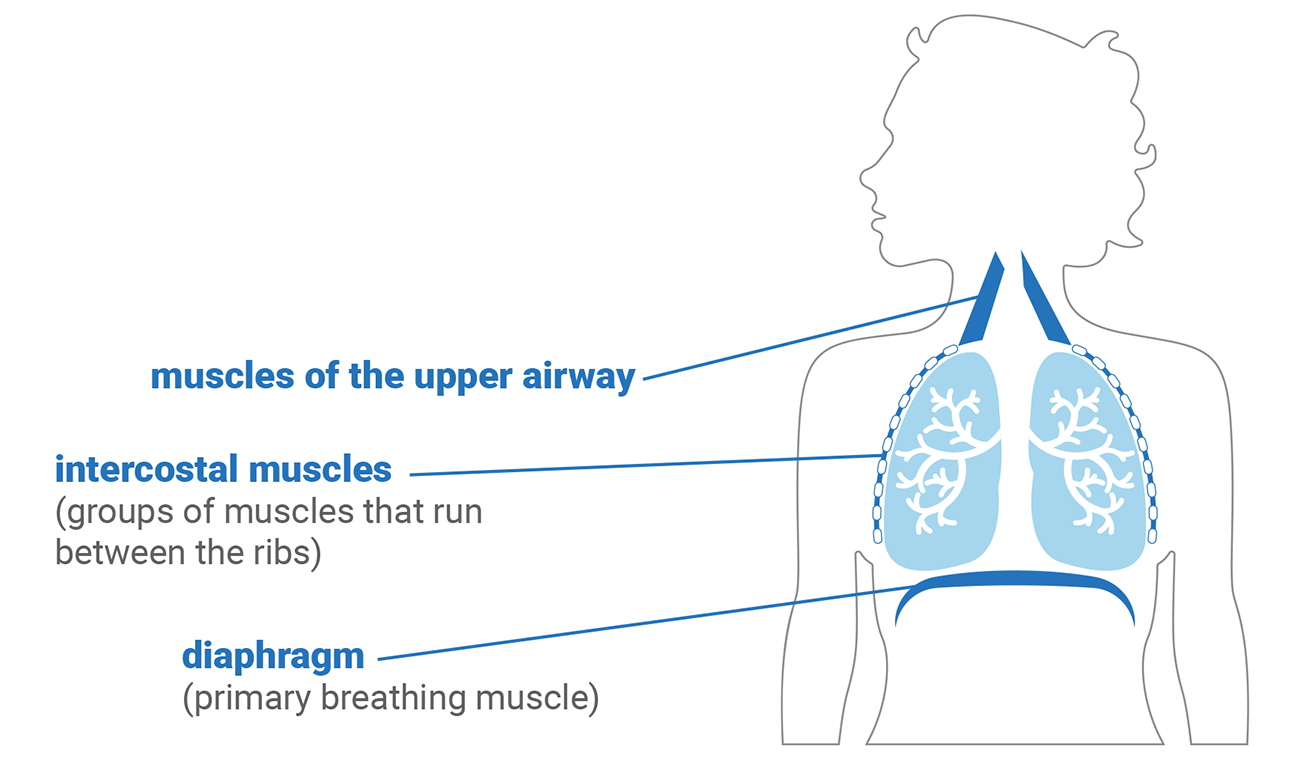
When you inhale...
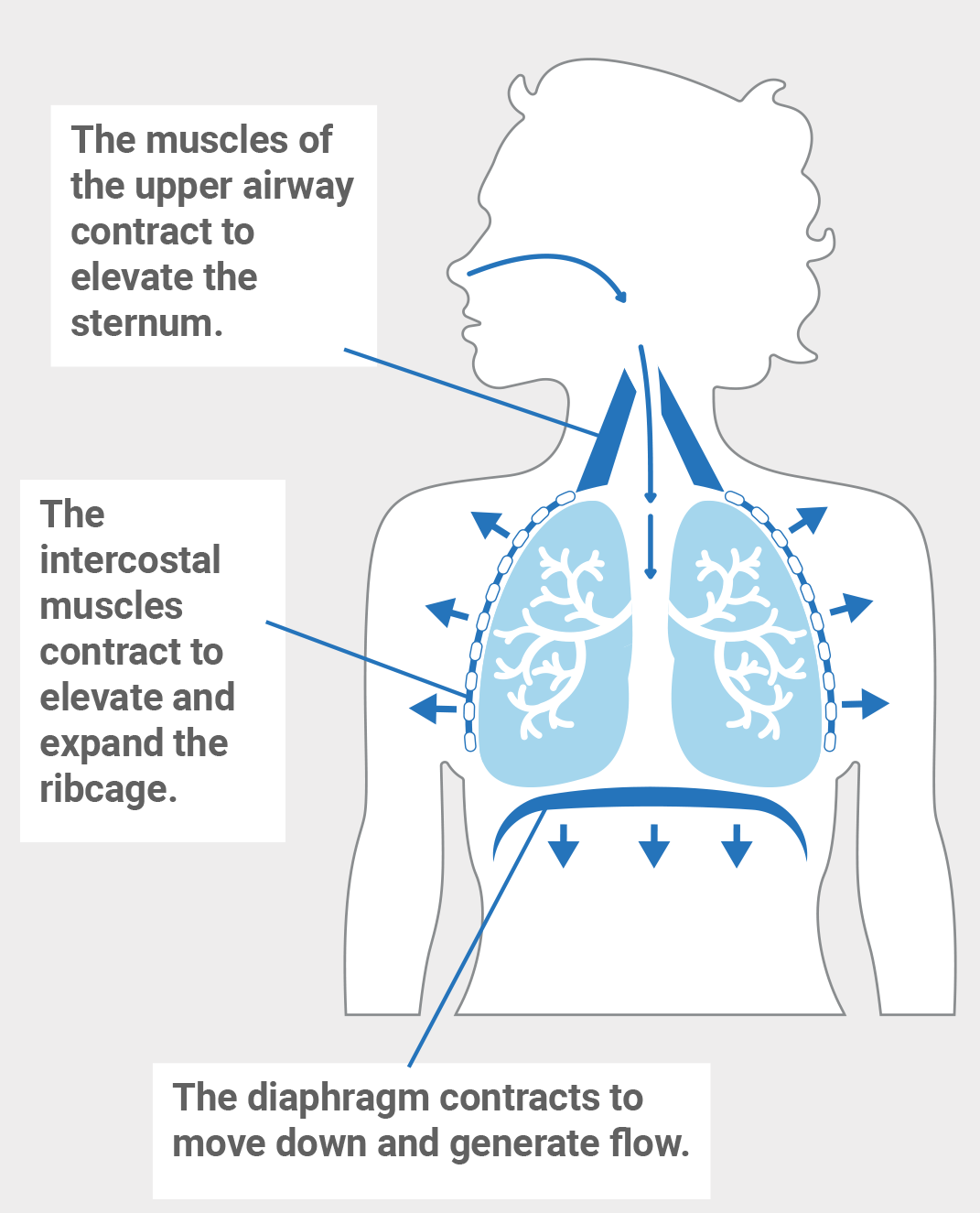
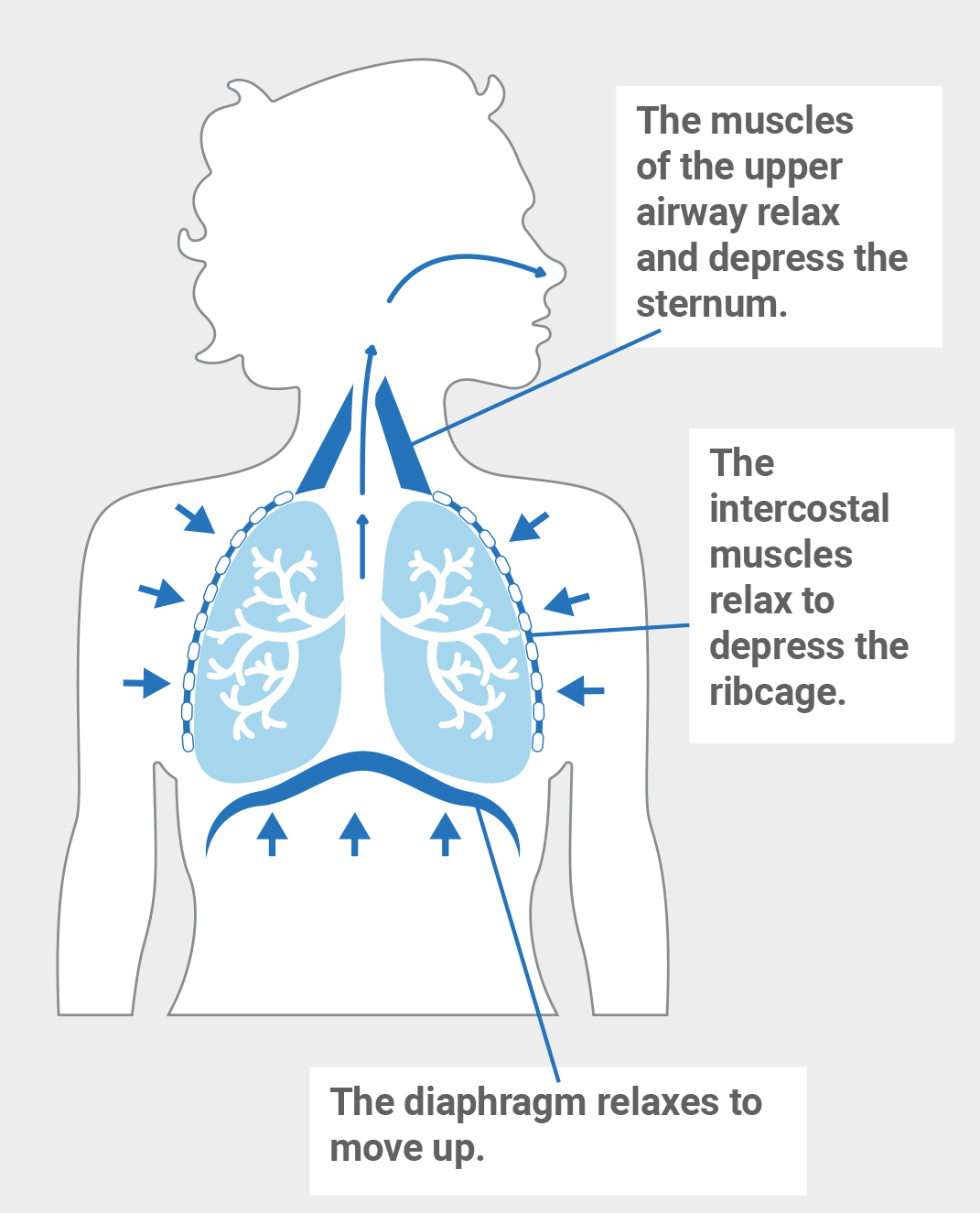
When you exhale...
Symptoms of respiratory muscle weakness










When ALS affects respiratory muscles, it results in “respiratory muscle weakness.”
People who have “respiratory muscle weakness” have lost strength in the muscles that help them breathe.
If you experience any of these symptoms, tell your ALS care team.
Breathing evaluations
Breathing test
What the breathing test measures
How the breathing test is done
Forced Vital Capacity (FVC)
Maximum inspiratory pressure (MIP)
Overnight oximetry

Arterial blood gas (ABG)

Sleep study
Oxygen and ALS
The muscles that control your breathing may be too weak to breathe in enough oxygen and breathe out enough carbon dioxide. Because of this, you may have higher than normal levels of carbon dioxide in your blood.
Your care team will usually recommend a “Non-invasive ventilation” or NIV (special breathing equipment). These machines help the respiratory muscles breathe in oxygen and breathe out carbon dioxide. If oxygen levels are still low, supplemental oxygen may be added to these machines with an order from a pulmonologist.
Using “supplemental” or extra oxygen will usually not help people living with ALS.
In fact, it can be very dangerous.
Supplemental oxygen can trick the brain into thinking that there is no need to breathe.
Mucus



Runny nose, oral care and extra saliva
How to reduce thin secretions in your nose
How to keep your mouth clean

How to remove extra saliva

Airway clearing devices

Your ALS Guide has short educational respiratory videos for you to learn more about equipment and managing respiratory symptoms.
YouTube Videos: bit.ly/als-respiration or youralsguide.com
Colds or respiratory viruses


Non-invasive therapies
People living with ALS may have trouble breathing while lying down flat. It might be helpful to use inclined support.
These could include:
- Breath stacking is a daily exercise that you can do to help open and expand your lungs.
- It is a way to fill your lungs with more air than you usually take in.
- It can be done with or without a device called an Ambu™ bag with a one-way valve.
- When breathing muscles weaken, the lungs get smaller. That makes it hard to breathe in enough oxygen and breathe out enough carbon dioxide.
- Breath stacking helps to keep the lungs open and the chest muscles flexible so you can breathe better.
- It also helps keep the lungs big and strong enough to remove secretions.

To do breath stacking, sit tall and take 3-5 slow, deep breaths from the mouth without exhaling. This should be done twice a day.
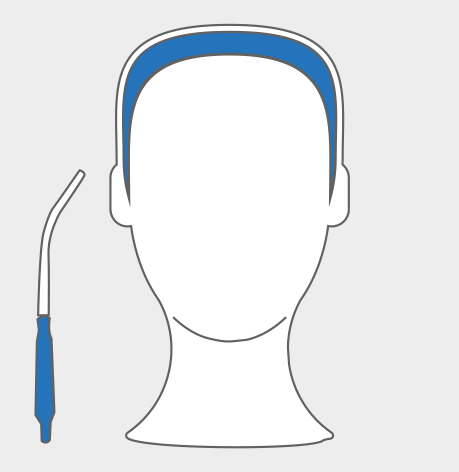
A nose clip can help make sure air doesn’t escape from the nose while you are breath-stacking.
If it is hard to breathe, an Ambu™ bag with a mask can help.
Watch this video, bit.ly/ambu-bag for instructions or ask your pulmonologist during a clinic visit about breath stacking.

Non-invasive ventilation
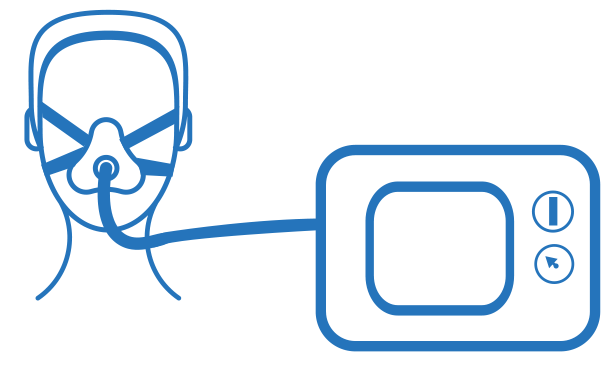
“Non-invasive ventilation” or NIV is the use of special equipment to support breathing. Non-invasive means that it does not break the skin or require any surgery. It is also the preferred and most used form of ventilation in ALS care.
People sometimes refer to non-invasive ventilation by other names. The most common ones are:
- BiPAP (Bi-level Positive Airway Pressure) machine
- VPAP (Variable Positive Airway Pressure) machine
- Home ventilator (portable with internal battery)
- When breathing muscles get weak and tired, NIV can help.
- The goal is to rest the respiratory muscles so that they don’t get too tired.
- Resting these muscles helps improve sleep, energy and communication.
- NIV may also help keep the body from collecting too much carbon dioxide if you don’t take enough breaths while sleeping.
- NIV may help people live longer with ALS.
NIV uses air pressure to help you breathe. Here’s how it works:
- You’ll wear a mask that’s attached to a device. There are a few different types of masks, so you can choose the one that’s most comfortable for you. Some masks cover just your nose, and others cover your mouth and your nose.
- When you wear the NIV device, it helps you get more air into your lungs, so you can breathe more easily.
- Some people use NIV all the time. Some people only use it at night or for short periods during the day. As your needs change, your ALS care team may recommend that you use NIV more often. Your care team may also change the amount of air pressure that you get through the NIV device.
Some of the available masks or interface options for NIV
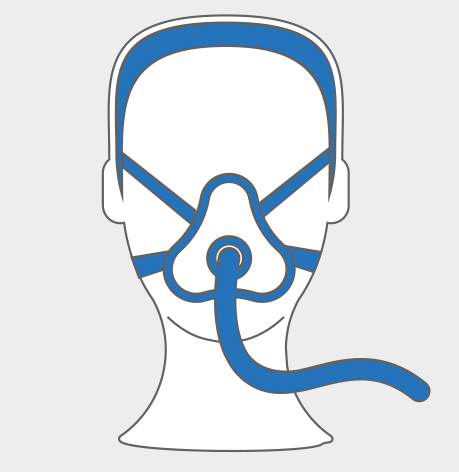

Talk with your ALS care team to choose the best option for you.
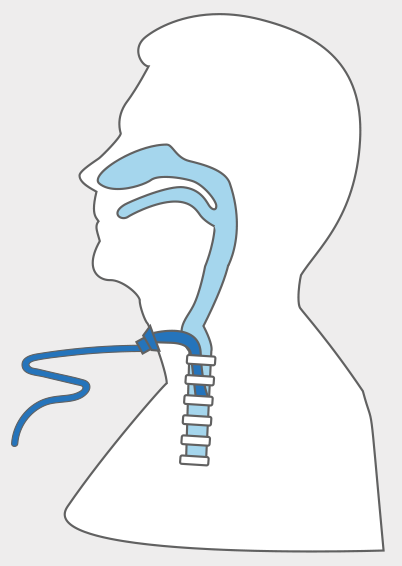
Invasive ventilation
You have the option to choose between non-invasive and invasive ventilation.
“Invasive” means that a doctor will do surgery to place a breathing tube inside your windpipe (trachea). This is called a tracheostomy.
- A tracheostomy is a surgical opening in the neck. A short tube is inserted into the throat. The tube keeps the airway open. Additional tubing connects the tracheostomy to a machine. A portable ventilator will breathe for you.
- The breathing machine blows air through the tube and into the lungs.
- Air from the lungs flows out through the tracheostomy opening in the throat, instead of through the nose or mouth.

You will most likely need to have a feeding tube placed. To learn more about feeding tubes visit, alsdecisions.org/nutrition.
- The tracheostomy is located below the vocal cords. Air movement across the vocal cords is required for speech. If possible, your doctor can adjust your machine settings to facilitate speech.
- You may not be able to speak or communicate in the same way that you did before the surgery.
- With today’s technology, you have options to communicate with the people who are most important to you.
- Your ALS care team can customize the best way for you to meet your communication needs.

Implications of invasive ventilation
Invasive ventilation support may drastically change how you are cared for and communicate. Therefore, this very personal decision should be discussed and considered thoroughly.
Give yourself time to consider how you want to live and experience the rest of your life. This decision impacts both you and your family in many ways, including financially and emotionally. Before a decision is made, advance directives should be in place.
If you have private health insurance and are considering invasive ventilation support, it is important to first contact your insurance company.
A person with invasive ventilation support requires 24-hour care from a caregiver, family member or nursing facility. Some insurance plans pay for an outside agency to provide part of this care.
Medicare does not pay for such services.
The tracheostomy site and equipment needs to be cleaned every day. This will help prevent lung infections.
Secretions from the lungs must be regularly cleared from the tube with a disposable suction catheter. This will help keep the airways open.
To find out more, visit youralsguide.com/invasivemechanical-ventilation
Removal of invasive ventilation
To be taken off invasive ventilation, you must first be evaluated by a physician. You will then be admitted to hospice for removal of ventilation and end-of life-care.
Removal from invasive ventilation may take place in the hospital or at an in-patient hospice unit. You would be given medications to ease any discomfort and make the final moments as peaceful as possible. After the invasive ventilation is disconnected, it may be minutes to hours before breathing ends completely.
Preparations for power outages

Travel

If traveling by air, the airline should be contacted before making a reservation.
- Non-invasive ventilation and other breathing equipment may be carried on the airplane. It does not count as a “carry-on” item.
- Airlines recommend having enough battery power to last for nearly double the flight time.
- If the use of a BiPAP/VPAP or home ventilator is required in flight, a back-up battery will be needed.
A car inverter can help when traveling or using respiratory devices in a car.

With or without the use of NIV or invasive ventilation, your ALS care team may recommend palliative or hospice care. Palliative care won’t help you live longer, but it can provide care and support to help you stay comfortable. Hospice care provides compassionate care and comfort at the end of life.
A palliative care provider or ALS care team can give you medicine to help with your symptoms, other equipment and recommend exercises to help with your breathing, posture and cough.
Talk to your ALS care team to figure out the right treatment plan for you.
Learn more
My ALS Decision Tool™
ALS Learning Series
My ALS Communication Passport to Quality Care
Support Groups
These resources are made possible by a generous donation from the Gilbert & Jacqueline Fern Foundation and other donors to the Foundation.
Sign up for News and Updates
Get helpful resources and updates from the Les Turner ALS Foundation delivered straight to your inbox. You’ll receive information on additional decision tools to help you understand your treatment options and make the decision that's right for you, plus information on upcoming events, ALS research, clinical trials, and more.