As researchers at the Les Turner ALS Center at Northwestern Medicine search for the root causes of ALS, they are examining processes within the body — even down to the cellular level.
In fact, recent research has shown that people living with ALS have abnormalities in their motor neuron’s cellular metabolism. Each cell has its own biochemical processes of energy production. But in people living with ALS and other neurodegenerative diseases, that basic function becomes dysfunctional.
The heart of metabolism within cells is mitochondria, which generates the energy needed to power the cell’s biochemical reactions.
 At Northwestern University’s Feinberg School of Medicine, Professor Navdeep Chandel is an expert in mitochondria. As the David W. Cugell, MD, Professor of Medicine and of Biochemistry and Molecular Genetics, he has studied mitochondria for decades, showing that it also plays an important role as a signaling molecule in the body.
At Northwestern University’s Feinberg School of Medicine, Professor Navdeep Chandel is an expert in mitochondria. As the David W. Cugell, MD, Professor of Medicine and of Biochemistry and Molecular Genetics, he has studied mitochondria for decades, showing that it also plays an important role as a signaling molecule in the body.
Chandel wondered whether this cellular metabolism dysfunction could be a driver of ALS or just a symptom of it. To find out, he set out to work with Evangelos Kiskinis, associate professor of neurology and neuroscience, to first define just how this metabolism changes within the motor neurons of people living with ALS.
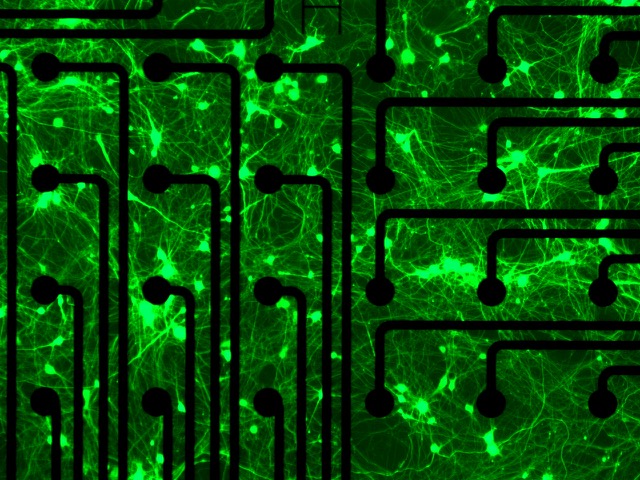
Armed with a grant from the Les Turner ALS Foundation, the pair and MD/PhD student Evan Kaspi began to work with Kiskinis’s induced pluripotent stem cell (iPSC) platform. These stem cells, derived from blood samples of people living with ALS patients, allow researchers to study motor neurons in detail to better understand why and how they die in ALS.
But from the start, Chandel noticed a problem. These stem cells were being kept alive in the lab in a special liquid called neurobasal medium. This liquid has been optimized to keep neurons thriving and healthy—a difficult task outside the body. But the medium is successful in part because it has high levels of glucose and does not actually mimic the environment inside the human body. Though this medium has been used for decades through the field, it posed a problem for Chandel. How could he study the role of mitochondria if the energy environment was so different?
Together, Chandel and Kiskinis decided to try to keep the motor neuron stem cells alive in a human plasma-like medium, which better mimicked conditions inside the human body. At first, the research team was concerned that the neurons might not even survive in this new medium.
“But they survived, and we found that their metabolic changes were very different than those in the neurobasal medium,” Chandel said.
Now, the team is working to define these metabolic changes, which could potentially lead to new therapies for the disease.
Robert Kalb, director of the Les Turner ALS Center at Northwestern Medicine, said research like this brings a new lens to the disease. “This team is studying two key aspects of cellular operations — how energy is produced and how damaged proteins are disposed of. Both of these processes are known to go awry in ALS,” he said. “Using human cells converted into motor neurons will bring a fresh perspective on what goes wrong in ALS.”
“This sort of research is high-risk, high-reward,” Chandel said. “I’m glad the Les Turner ALS Foundation was willing to take a risk on someone who doesn’t know a lot about ALS but who got together with a stem cell expert to bring in new energy to this area of research. With ALS, we don’t know the rules of the game. But if we figure out basic biology questions like this, it could help us figure out other neurodegenerative diseases, like Parkinson’s and Alzheimer’s, as well.”
Explore More Research at the Les Turner ALS Center