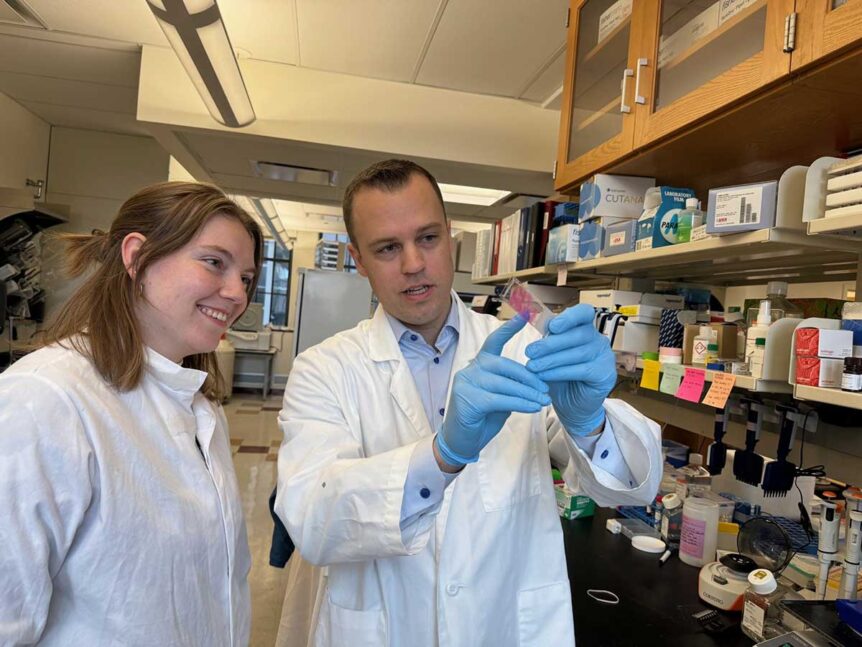
Using cutting-edge techniques, researchers at the Les Turner ALS Center at Northwestern Medicine are working to test an innovative hypothesis: that the immune system is involved in the breakdown of the connection between the brain and muscles in people with ALS.
“That’s still very much a hypothesis,” said David Gate, assistant professor of neurology at Northwestern’s Feinberg School of Medicine who leads the research. “In every neurodegenerative disease, the immune system is involved in some way. But there hasn’t been enough investigation into what the immune system is doing to the muscles that are wasting in ALS patients.”
 Gate is trying to do just that. The theory stems from the fact that most common genetic cause of inherited ALS is a genetic aberration called the C9orf72 repeater expansion. Researchers in the field have found that when the C9orf72 gene is eliminated in mice, their immune system becomes dysfunctional (even though many of the mice do not develop ALS).
Gate is trying to do just that. The theory stems from the fact that most common genetic cause of inherited ALS is a genetic aberration called the C9orf72 repeater expansion. Researchers in the field have found that when the C9orf72 gene is eliminated in mice, their immune system becomes dysfunctional (even though many of the mice do not develop ALS).
Previous research has shown that people with the inherited form of ALS have specific immune changes in their blood. A certain kind of first-line immune cell called a monocyte becomes dysfunctional.
“It’s possible that these immune system changes are influencing an ALS patient’s ability to fend off infections, but it’s also possible that this immune system component might be responsible for the variability in the severity of the disease,” Gate said. “It could actually be causing or participating in symptoms.”
Even those living with the sporadic form of ALS, who do not have the genetic aberration, experience immune changes, Gate said, so it’s possible his research could extend to better understand that form of the disease, as well.
With a grant from the Les Turner ALS Foundation, he genetically sequenced every immune cell in blood samples from people with the inherited form of ALS. He also sequenced immune cells from control patients. The grant gave him the preliminary data he needed to receive more grants to continue the research.
Next, he is working with Evangelos Kiskinis, associate professor of neurology and neuroscience at the Feinberg School of Medicine, to profile those cells in the brain and spinal cords from deceased donors who had ALS. “Now we are trying to connect the dots between the blood immune response and the tissue immune response,” he said.
This idea of “neuroimmunology” has been well studied in other neurodegenerative diseases, like Alzheimer’s, but Gate estimates that this sort of research with ALS is 15 years behind that. “People are now starting to appreciate the involvement of the immune system in ALS,” he said. “It’s picking up steam in the field.”
“Over the past several years the scientific community has paid increasing attention to the ‘cellular neighborhood’ as a driver of motor neuron death in ALS,” said Robert Kalb, director of the Les Turner ALS Center at Northwestern Medicine. “Using state-of-the-art approaches, David is investigating the contributions of immune cells and, in particular, molecularly distinct types of immune cells, to motor neuron death in ALS. I look forward to seeing where these results lead.”
For Gate, who joined Northwestern in 2021 specifically to be a part of one of the largest ALS clinics in the world, this early support from the Les Turner ALS Foundation helped jumpstart his research here and will hopefully help lead to new treatments. “Understanding how the immune system is connected to ALS patients can also help inform how to treat individual patients,” he said.